![]()
Dr. Christopher W. Kerr is the Chief Medical Officer at The Center for Hospice and Palliative Care in Buffalo, New York, where he has worked since 1999. His background in research has evolved from bench science towards the human experience of illness as witnessed from the bedside, specifically patients’ dreams and visions at the end of life. Although medically ignored, these near universal experiences often provide comfort and meaning as well as insight into the life led and the death anticipated.
To learn more about death bed visions, shared death experiences, after death communications, and related phenomenon, go here.
To learn more about the power of dreams and dreaming, go here.
…………
…………
What Deathbed Visions Teach Us About Living
By Phoebe Zerwick
DNYUZ
March 12, 2024
Chris Kerr was 12 when he first observed a deathbed vision. His memory of that summer in 1974 is blurred, but not the sense of mystery he felt at the bedside of his dying father. Throughout Kerr’s childhood in Toronto, his father, a surgeon, was too busy to spend much time with his son, except for an annual fishing trip they took, just the two of them, to the Canadian wilderness. Gaunt and weakened by cancer at 42, his father reached for the buttons on Kerr’s shirt, fiddled with them and said something about getting ready to catch the plane to their cabin in the woods. “I knew intuitively, I knew wherever he was, must be a good place because we were going fishing,” Kerr told me.
As he moved to touch his father, Kerr felt a hand on his shoulder. A priest had followed him into the hospital room and was now leading him away, telling him his father was delusional. Kerr’s father died early the next morning.Kerr now calls what he witnessed an end-of-life vision. His father wasn’t delusional, he believes. His mind was taking him to a time and place where he and his son could be together, in the wilds of northern Canada. And the priest, he feels, made a mistake, one that many other caregivers make, of dismissing the moment as a break with reality, as something from which the boy required protection.
It would be more than 40 years before Kerr felt compelled to speak about that evening in the hospital room. He had followed his father, and three generations before him, into medicine and was working at Hospice & Palliative Care Buffalo, where he was the chief medical officer and conducted research on end-of-life visions. It wasn’t until he gave a TEDx Talk in 2015 that he shared the story of his father’s death. Pacing the stage in the sport coat he always wears, he told the audience: “My point here is, I didn’t choose this topic of dying. I feel it has chosen or followed me.” He went on: “When I was present at the bedside of the dying, I was confronted by what I had seen and tried so hard to forget from my childhood. I saw dying patients reaching and calling out to mothers, and to fathers, and to children, many of whom hadn’t been seen for many years. But what was remarkable was so many of them looked at peace.”
The talk received millions of views and thousands of comments, many from nurses grateful that someone in the medical field validated what they have long understood. Others, too, posted personal stories of having witnessed loved ones’ visions in their final days. For them, Kerr’s message was a kind of confirmation of something they instinctively knew — that deathbed visions are real, can provide comfort, even heal past trauma. That they can, in some cases, feel transcendent. That our minds are capable of conjuring images that help us, at the end, make sense of our lives.
Nothing in Kerr’s medical training prepared him for his first shift at Hospice Buffalo one Saturday morning in the spring of 1999. He had earned a degree from the Medical College of Ohio while working on a Ph.D. in neurobiology. After a residency in internal medicine, Kerr started a fellowship in cardiology in Buffalo. To earn extra money to support his wife and two young daughters, he took a part-time job with Hospice Buffalo. Until then, Kerr had worked in the conventional medical system, focused on patients who were often tethered to machines or heavily medicated. If they recounted visions, he had no time to listen. But in the quiet of Hospice, Kerr found himself in the presence of something he hadn’t seen since his father’s death: patients who spoke of people and places visible only to them. “So just like with my father, there’s just this feeling of reverence, of something that wasn’t understood but certainly felt,” he says.
During one of his shifts, Kerr was checking on a 70-year-old woman named Mary, whose grown children had gathered in her room, drinking wine to lighten the mood. Without warning, Kerr remembers, Mary sat up in her bed and crossed her arms at her chest. “Danny,” she cooed, kissing and cuddling a baby only she could see. At first, her children were confused. There was no Danny in the family, no baby in their mother’s arms. But they could sense that whatever their mother was experiencing brought her a sense of calm. Kerr later learned that long before her four children were born, Mary lost a baby in childbirth. She never spoke of it with her children, but now she was, through a vision, seemingly addressing that loss.
In observing Mary’s final days at Hospice, Kerr found his calling. “I was disillusioned by the assembly-line nature of medicine,” Kerr told me. “This felt like a more humane and dignified model of care.” He quit cardiology to work full time at the bedsides of dying patients. Many of them described visions that drew from their lives and seemed to hold meaning, unlike hallucinations resulting from medication, or delusional, incoherent thinking, which can also occur at the end of life. But Kerr couldn’t persuade other doctors, even young residents making the rounds with him at Hospice, of their value. They wanted scientific proof.
At the time, only a handful of published medical studies had documented deathbed visions, and they largely relied on secondhand reports from doctors and other caregivers rather than accounts from patients themselves. On a flight home from a conference, Kerr outlined a study of his own, and in 2010, a research fellow, Anne Banas, signed on to conduct it with him. Like Kerr, Banas had a family member who, before his death, experienced visions — a grandfather who imagined himself in a train station with his brothers.
The study wasn’t designed to answer how these visions differ neurologically from hallucinations or delusions. Rather, Kerr saw his role as chronicler of his patients’ experiences. Borrowing from social-science research methods, Kerr, Banas and their colleagues based their study on daily interviews with patients in the 22-bed inpatient unit at the Hospice campus in the hope of capturing the frequency and varied subject matter of their visions. Patients were screened to ensure that they were lucid and not in a confused or delirious state. The research, published in 2014 in The Journal of Palliative Medicine, found that visions are far more common and frequent than other researchers had found, with an astonishing 88 percent of patients reporting at least one vision. (Later studies in Japan, India, Sweden and Australia confirm that visions are common. The percentages range from about 20 to 80 percent, though a majority of these studies rely on interviews with caregivers and not patients.)
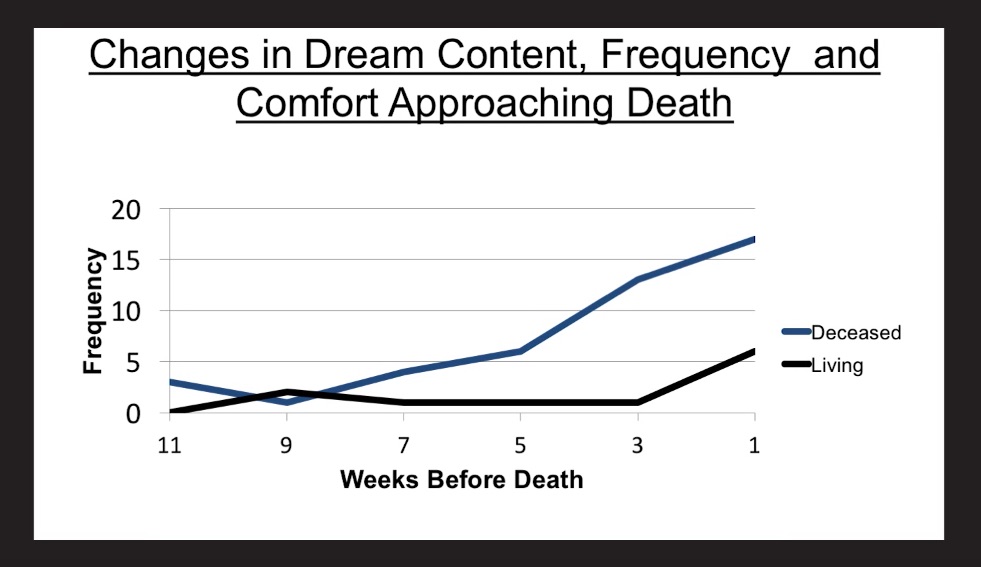
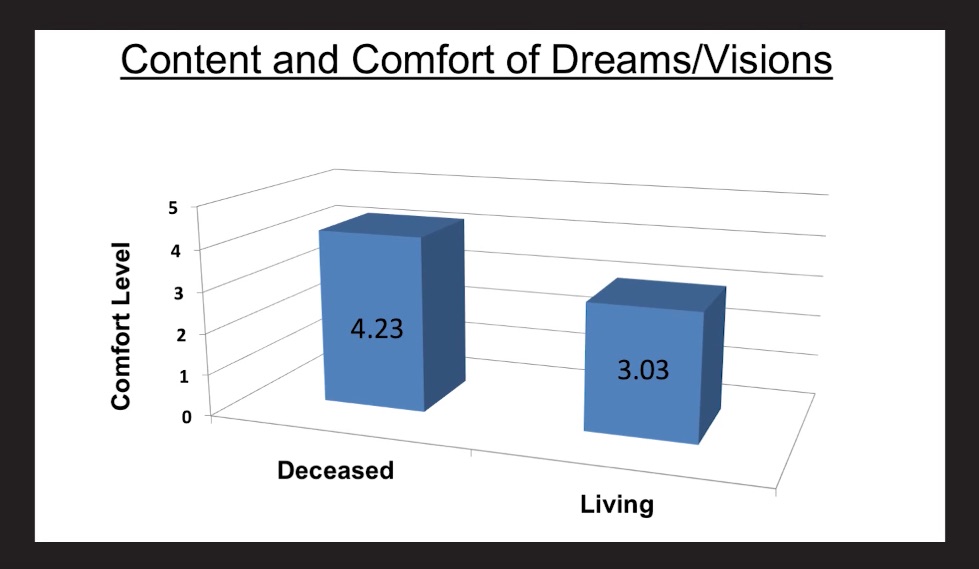
In the last 10 years, Kerr has hired a permanent research team who expanded the studies to include interviews with patients receiving hospice care at home and with their families, deepening the researchers’ understanding of the variety and profundity of these visions. They can occur while patients are asleep or fully conscious. Dead family members figure most prominently, and by contrast, visions involving religious themes are exceedingly rare. Patients often relive seminal moments from their lives, including joyful experiences of falling in love and painful ones of rejection. Some dream of the unresolved tasks of daily life, like paying bills or raising children. Visions also entail past or imagined journeys — whether long car trips or short walks to school. Regardless of the subject matter, the visions, patients say, feel real and entirely unique compared with anything else they’ve ever experienced. They can begin days, even weeks, before death. Most significant, as people near the end of their lives, the frequency of visions increases, further centering on deceased people or pets. It is these final visions that provide patients, and their loved ones, with profound meaning and solace.
Kerr’s latest research is focused on the emotional transformation he has often observed in patients who experience such visions. The first in this series of studies, published in 2019, measured psychological and spiritual growth among two groups of hospice patients: those who had visions and a control group of those who did not. Patients rated their agreement with statements including, “I changed my priorities about what is important in life,” or “I have a better understanding of spiritual matters.” Those who experienced end-of-life visions agreed more strongly with those statements, suggesting that the visions sparked inner change even at the end of life. “It’s the most remarkable of our studies,” Kerr told me. “It highlights the paradox of dying, that while there is physical deterioration, they are growing and finding meaning. It highlights what patients are telling us, that they are being put back together.”
In the many conversations Kerr and I have had over the past year, the contradiction between medicine’s demand for evidence and the ineffable quality of his patients’ experiences came up repeatedly. He was first struck by this tension about a year before the publication of his first study, during a visit with a World War II veteran named John who was tormented throughout his life by nightmares that took him back to the beaches of Normandy on D-Day. John had been part of a rescue mission to bring wounded soldiers to England by ship and leave those too far gone to die. The nightmares continued through his dying days, until he dreamed of being discharged from the Army. In a second dream, a fallen soldier appeared to John to tell him that his comrades would soon come to “get” him. The nightmares ended after that.
Kerr has been nagged ever since by the inadequacy of science, and of language, to fully capture the mysteries of the mind. “We were so caught up in trying to quantify and give structure to something so deeply spiritual, and really, we were just bystanders, witnesses to this,” he says. “It feels a little small to be filling in forms when you’re looking at a 90-something-year-old veteran who is back in time 70 years having an experience you can’t even understand.” When Kerr talks about his research at conferences, nurses tend to nod their heads in approval; doctors roll their eyes in disbelief. He finds that skeptics often understand the research best when they watch taped interviews with patients.
What’s striking about this footage, which dates back to Kerr’s early work in 2008, is not so much the content of the visions but rather the patients’ demeanor. “There’s an absence of fear,” Kerr says. A teenage girl’s face lights up as she describes a dream in which she and her deceased aunt were in a castle playing with Barbie dolls. A man dying of cancer talks about his wife, who died several years earlier and who comes to him in his dreams, always in blue. She waves. She smiles. That’s it. But in the moment, he seems to be transported to another time or place.
Kerr has often observed that in the very end, dying people lose interest in the activities that preoccupied them in life and turn toward those they love. As to why, Kerr can only speculate. In his 2020 book, “Death Is but a Dream,” he concludes that the love his patients find in dying often brings them to a place that some call enlightenment and others call God. “Time seems to vanish,” he told me. “The people who loved you well, secured you and contributed to who you are are still accessible at a spiritual and psychological level.”
That was the case with Connor O’Neil, who died at the age of 10 in 2022 and whose parents Kerr and I visited in their home. They told us that just two days before his death, their son called out the name of a family friend who, without the boy’s knowledge, had just died. “Do you know where you are?” Connor’s mother asked. “Heaven,” the boy replied. Connor had barely spoken in days or moved without help, but in that moment, he sat up under his own strength and threw his arms around her neck. “Mommy, I love you,” he said.
Kerr’s research finds that such moments, which transcend the often-painful physical decline in the last days of life, help parents like the O’Neils and other relatives grieve even unfathomable loss. “I don’t know where I would be without that closure, or that gift that was given to us,” Connor’s father told us. “It’s hard enough with it.” As Kerr explains, “It’s the difference between being wounded and soothed.”
In June, I visited the adult daughter of a patient who died at home just days earlier. We sat in her mother’s living room, looking out on the patio and bird feeders that had given the mother so much joy. Three days before her mother’s death, the daughter was straightening up the room when her mother began to speak more lucidly than she had in days. The daughter crawled into her mother’s bed, held her hand and listened. Her mother first spoke to the daughter’s father, whom she could see in the far corner of the room, handsome as ever. She then started speaking with her second husband, visible only to her, yet real enough for the daughter to ask whether he was smoking his pipe. “Can’t you smell it?” her mother replied. Even in the retelling, the moment felt sacred. “I will never, ever forget it,” the daughter told me. “It was so beautiful.”
I also met one of Banas’s patients, Peggy Haloski, who had enrolled in hospice for home care services just days earlier, after doctors at the cancer hospital in Buffalo found blood clots throughout her body, a sign that the yearlong treatment had stopped working. It was time for her husband, Stephen, to keep her comfortable at home, with their two greyhounds.
Stephen led Banas and me to the family room, where Peggy lay on the couch. Banas knelt on the floor, checked her patient’s catheter, reduced her prescriptions so there were fewer pills for her to swallow every day and ordered a numbing cream for pain in her tailbone. She also asked about her visions.
The nurse on call that weekend witnessed Peggy speaking with her dead mother.
“She was standing over here,” Peggy told Banas, gesturing toward the corner of the room.
“Was that the only time you saw her?” Banas asked.
“So far.”
“Do you think you’ll be seeing her more?”
“I will. I will, considering what’s going on.”
Peggy sank deeper into the couch and closed her eyes, recounting another visit from the dead, this time by the first greyhound she and Stephen adopted. “I’m at peace with everybody. I’m happy,” she said. “It’s not time yet. I know it’s not time, but it’s coming.”
When my mother, Chloe Zerwick, was dying in 2018, I had never heard of end-of-life visions. I was acting on intuition when her caregivers started telling me about what we were then calling hallucinations. Mom was 95 and living in her Hudson Valley home under hospice care, with lung disease and congestive heart failure, barely able to leave her bed. The hospice doctor prescribed an opioid for pain and put her on antipsychotic and anti-anxiety medicines to tame the so-called hallucinations he worried were preventing her from sleeping. It is possible that some of these medications caused Mom’s visions, but as Kerr has explained, drug-induced hallucinations do not rule out naturally occurring visions. They can coexist.
In my mother’s case, I inherently understood that her imaginary life was something to honor. I knew what medicine-induced hallucinations looked and felt like. About 10 years before her death, Mom fell and injured her spine. Doctors in the local hospital put her on an opioid to control the pain, which left her acting like a different person. There were spiders crawling on the hospital wall, she said. She mistook her roommate’s bed for a train platform. Worse, she denied that I loved her or ever did. Once we took her off the medicine, the hallucinations vanished.
The visions she was having at the end of her life were entirely different; they were connected to the long life she had led and brought a deep sense of comfort and delight. “You know, for the first time in my life I have no worries,” she told me. I remember feeling a weight lift. After more than a decade of failing health, she seemed to have found a sense of peace.
The day before her death, as her breathing became more labored, Mom made an announcement: “I have a new leader,” she said.
“Who is that?” I asked.
“Mark. He’s going to take me to the other side.”
She was speaking of my husband, alive and well back home in North Carolina.
“That’s great, Mom, except that I need him here with me,” I replied. “Do you think he can do both?”
“Oh, yes. He’s very capable.”
That evening, Mom was struggling again to breathe. “I’m thinking of the next world,” she said, and of my husband, who would lead her there. The caregiver on duty for the night and I sat at her bedside as Mom’s oxygen level fell from 68 to 63 to 52 and kept dropping until she died the next morning. My mother was not a brave person in the traditional sense of the word. She was afraid of snakes, the subway platform and any hint of pain. But she faced her death, confident that a man who loves her daughter would guide her to whatever lay ahead.
“Do you think it will happen to you?” she asked me at one point about her dreaming life.
“Maybe it’s genetic,” I replied, not knowing, as I do now, that these experiences are part of what may await us all.
…………
End Of Life Dreams Studied At Hospice Buffalo
WIVB
November 8, 2019
Hospice Buffalo is gaining worldwide attention for years of study involving the vivid dreams that dying patients report having in their final days of life.
“Everybody I knew that was dead was there,” said the late Jeanne Faber, a former patient of Hospice Buffalo who is one of hundreds of patients who Hospice Buffalo interviewed on video shortly before her death about her very vivid end of life dreams.
She says the dreams became more frequent the sicker she became. “I have seen my mother, recently more. “I can’t say that my mother and I got along all those years, but we made up for it in the end,” said Faber.
“As soon as I started here, this seemed to be common knowledge among people who work with dying patients and who were closer to the bedside,” said Dr, Christopher Kerr, CEO of Hospice Buffalo. “I ended up studying it because as I came to appreciate that there was this kind of subjective or non-physical element to dying, that it was important an inherently therapeutic.”
The late Paul Schaefer reported dreaming about his late wife several times after she passed years ago. “She always kind of let me know that she’s fine. I get that feeling after a dream like that,” said Schaefer, who notes that the last one he had shortly before his death was different. “She wanted me to pack up some things for her, so I had this crazy dream I’m packing goods and I’m setting them for some reason up high, and everything went fine until I fell out of bed ha ha, and I really clunked.”
Paul died a few weeks after that interview with Hospice Buffalo researchers
In the final days of life, dreams seem to bring comfort and tie up loose ends, according to Dr. Kerr. “The thing you have to realize is the time for therapy and analysis is over. They’re nearing the end of their lives and people aren’t emerging from these experiences with questions; ‘what happened to me?’ They’re coming out of this with answers and meaning.”
The late Maggie Scheelar is convinced she saw her deceased sister. “So, I said Beth, you gotta stay with me. I’m alone, stay. And she says, I can’t, not now. Then she says ‘Soon we’ll be back, we’ll be together.”
Dr. Kerr does not believe it has anything to do with pain killing drugs or hallucinations. “We ruled out people who had confusional states. So these people are cognitively in tact.”
Hospice Buffalo researchers haven’t been focused on WHY these end of life dreams happen, but more on the fact that they DO happen with great frequency, and the hope that the rest of the medical world should not be so quick to dismiss end-of-life dreams.
“This was a very significant thing, but when I woke up, I was happy. It left me with a good feeling,” said Faber, who didn’t just dream about her pre-deceased relatives, but also the dog she missed. “Because she was a blind dog and I took care of her for so many years. I just lost her a year ago. All I could see her was running the fields…and not being blind anymore.”
“Personally, I just think it’s better story than the one we might think we’re seeing,” said Dr. Kerr. “Those things that we’ve truly loved and cherished are never really gone.”
Not only do these end of life dreams seem to help those dying, but also the loved ones they leave behind.
“In my opinion it’s real. To them, it’s real,” said Tammy, the mother of a Hospice Buffalo patient who experienced a comforting end of life dream.
Sue Olesky noticed how dreams brought her mother comfort before death. “She didn’t even talk about them as dreams. To her, they were something that happened last night,” said Olesky.
Norb misses his late wife, a former Hospice Buffalo patient. “But knowing how she died, what mood she was in when she died has put me at great ease over it, really.”
A documentary about this research recently won an award at the Barcelona Film Festival. A book about this research, titled, “Death is but a Dream” comes out in February, and ten countries have bought copies in advance. Netflix is also doing a full episode about this research next fall.
…………
Who You See Before You Die: Hospice Documenting Patients’ Mysterious Dream Experiences
By David Highfield
KDKA
February 25, 2019
Death is one of the mysteries of life. But the dreams of patients at Hospice Buffalo in New York State are revealing something incredible about the process of dying.
Dr. Christopher Kerr and his team have been documenting dreams or visions of dying patients for years.
They’ve found that the dreams are often comforting and make death less scary.
It turns out, when we have little time left, many of us may see the people we miss the most.
They’ve recorded many of the interviews.
A man named Horace explained one of his dreams: “My wife all of a sudden appeared.”
A woman named Jeanne describes how vivid they are: “I remember seeing every piece of their face. I mean, I know that was my mom and dad and uncle and my brother-in-law.” She continued: “I felt good. I felt good to see some people.”
A patient named Maggie dreamt about her sister, who had passed away before her.
“So I said, Beth, you’ve got to stay with me,” Maggie said. “I’m alone, stay with me. She says, ‘I can’t. Not now.”
But then, her sister gives her a message: “And then she says, ‘Soon we’ll be back. We’ll be back together.”
Dr. Kerr didn’t start out believing. He’s now the Chief Medical Officer at Hospice Buffalo, and when he was first starting out, something happened that opened his mind. He thought a certain patient could live a little longer with IV fluids.
“I walked in and the nurse didn’t even look up,” said Dr. Kerr. “And she said, “No, no, he’s dying,’ and I said, ‘Why are you saying that?’ And she said, ‘Well, he’s seeing his deceased mother,’ and I was like [laughing noise] ‘Yeah, right.’”
He was skeptical, but he explained that he was proven wrong over and over.
“Everybody but me was able to prognosticate death in part based on what people were seeing or experiencing,” he said.
He says doctors aren’t trained to deal with these dreams, but he began studying them and realized that they’re therapeutic.
“Instead of having this fear of death,” said Dr. Kerr. “It almost transcends the fear of death to something bigger.”
In 10 years, he and his team have documented 14,000 cases. Eighty percent of his patients report dreams or visions.
“What’s clear is people are universally saying this feels more real and different than any dream I’ve ever had before,” he said.
KDKA met one of those patients during our visit, a man named Gregg Liebler.
Liebler: “My grandmother and grandfather are both passed.”
Dr. Kerr: “Have you had any dreams of them?”
Liebler: “Yes. I see them often.”
Liebler’s sister, Karen Paciorkowski, is a nurse at Hospice Buffalo.
“He was really close with my mom’s parents,” she said.
“The people who loved him and nurtured him, he says the most, were his grandparents and that’s who returns to him,” Dr. Kerr said.
He sees himself as a child, talking to them again.
Dr. Kerr: “But it feels good?”
Liebler: “It sure does.”
Liebler passed away less than three weeks after our interview.
“You’re physically declining, but inside, you’re very vibrant and alive,” said Dr. Kerr.
He says the dreams happen more often as death gets closer, and there are common themes, like upcoming travel.
A patient named Paul shared one of his dreams, “She wanted me to pack up some things for her, so I had this crazy dream, I’m packing goods.”
Sometimes the dreams allow people to address unresolved issues.
A patient named Patricia felt relief after delivering a message to her deceased husband: “I told him, ‘You should have taken care of this, and I want you to know that I’m really angry that you didn’t,’ and he smiled.”
When children are dying, they often don’t know any people who have passed, so they dream of deceased pets.
A girl named Jessica explains her dreams: “I dream about my old dog Shadow, that has passed away.”
“They’ll come of these experiences and say they want to go back,” said Dr. Kerr.
So what causes the dreams? Is there a religious, spiritual or scientific explanation?
“I don’t have one,” said Dr. Kerr.
He says his goal is just to record what’s happening and he’s not sure there need to be an explanation.
“When they wake up crying because they’ve been so deeply moved by something,” said Dr. Kerr. “That just should be respected. Period.”